A 54-year-old male with a medical history of hypertension and GERD presents to the GI clinic with a chief complaint of dysphagia for six months. It is intermittent and only to solids, most commonly when eating beef or chicken. He estimates symptoms occur one to two times per month. This has remained stable over the last six months with no progression. He denies dysphagia to liquids or soft food. He has not lost weight. He denies nausea, vomiting, melena, hematemesis or coffee ground emesis.
His GERD is well controlled by 20 mg daily of omeprazole taken orally 30 minutes prior to breakfast. His hypertension is well controlled by lisinopril. He does not take any other medications, including over-the-counter products or supplements. He has no history of asthma, seasonal allergies or food allergies. There is no known family history of gastrointestinal malignancy.
Nine months ago, at his annual primary care evaluation, routine lab tests were completed, including complete blood count and comprehensive metabolic panels. Results were all within normal limits. His physical examination is unremarkable. Specifically, there was no evidence of lymphadenopathy, thyromegaly, or palpable masses or tenderness in the chest or abdomen during the examination.

A 54-year-old male with a medical history of hypertension and GERD presents to the GI clinic with a chief complaint of dysphagia for six months. It is intermittent and only to solids, most commonly when eating beef or chicken. He estimates symptoms occur one to two times per month. This has remained stable over the last six months with no progression. He denies dysphagia to liquids or soft food. He has not lost weight. He denies nausea, vomiting, melena, hematemesis or coffee ground emesis.
His GERD is well controlled by 20 mg daily of omeprazole taken orally 30 minutes prior to breakfast. His hypertension is well controlled by lisinopril. He does not take any other medications, including over-the-counter products or supplements. He has no history of asthma, seasonal allergies or food allergies. There is no known family history of gastrointestinal malignancy.
Nine months ago, at his annual primary care evaluation, routine lab tests were completed, including complete blood count and comprehensive metabolic panels. Results were all within normal limits. His physical examination is unremarkable. Specifically, there was no evidence of lymphadenopathy, thyromegaly, or palpable masses or tenderness in the chest or abdomen during the examination.
What is most likely the cause of his dysphagia?
A) Pill-induced esophagitis
B) Malignant stricture secondary to adenocarcinoma
C) Schatzki ring
D) Zenker’s diverticulum
The correct answer is C, Schatzki ring.
Practice Pearls
*Esophageal rings are narrow bands of tissue that can partially obstruct the esophageal lumen.
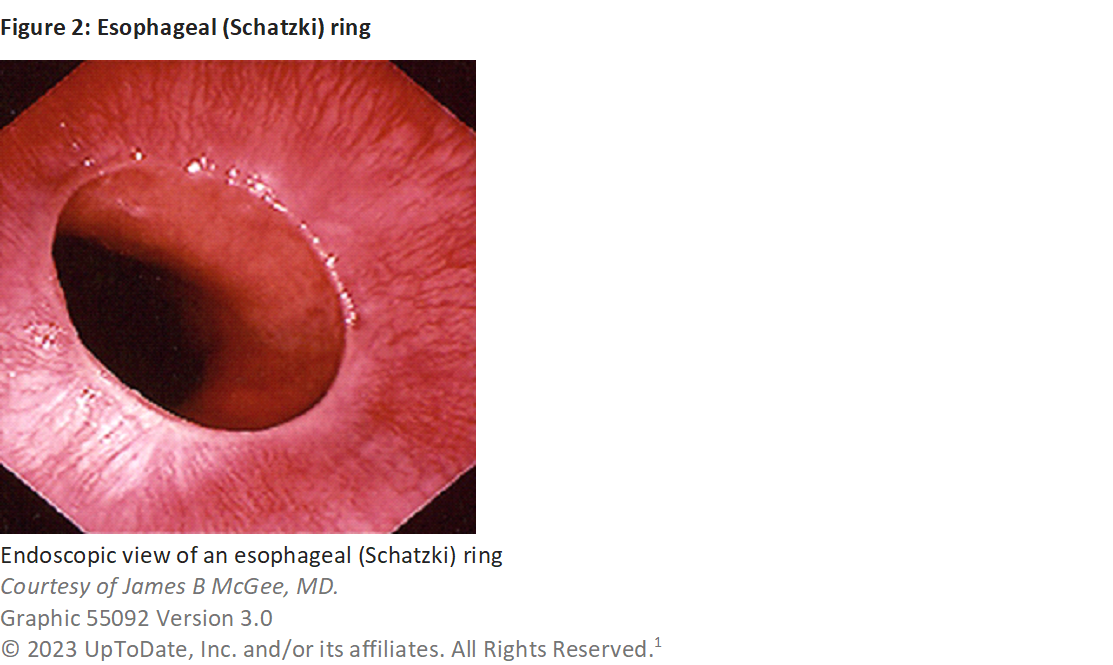
*Schatzki ring, also known as a B ring, is a mucosal structure precisely at the squamocolumnar junction.1 It is smooth and thin (< 5 mm in axial length) and covered with squamous mucosa proximally and columnar epithelium distally.1
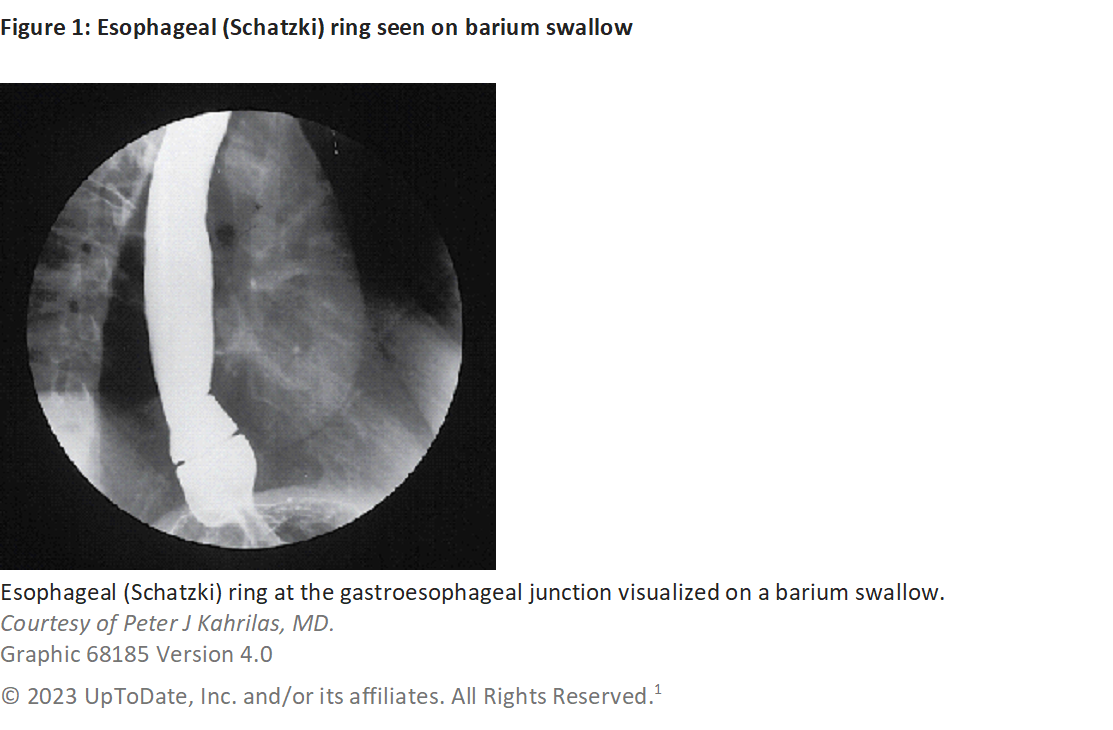
*The true prevalence of Schatzki ring is unknown. Schatzki rings are found in six to 14 percent of routine barium esophagrams for dysphagia (Image 1).1 They have been identified in up to 13 percent of patients undergoing upper endoscopy (Image 2).1
*The pathogenesis is unknown. It is hypothesized that Schatzki rings are secondary to chronic damage from GERD.2 A congenital or developmental origin has also been proposed.
Associated Conditions and Clinical Presentation
*Schatzki rings are almost always associated with hiatal hernias and can be associated with eosinophilic esophagitis.
*Schatzki rings are nonhereditary but may be associated with conditions that could have a hereditary predisposition, such as Barrett’s esophagus.
*Most patients are asymptomatic. Those with symptoms present with intermittent, nonprogressive dysphagia to solids. Most often, they will report difficulty with hard dry foods like meats or breads.
*Key questions to ask include the location of discomfort in swallowing, which would be expected to be subxiphoid (lower chest/upper abdominal area), and whether symptoms occur with solids, liquids or both.
*The presence and severity of symptoms depends on the internal diameter of the esophageal lumen. Patients with an esophageal lumen < 13 mm (39 French) will often experience solid food dysphagia.
*Occasionally, patients present with an acute onset of dysphagia or complete inability to swallow saliva due to food impaction. These patients should be referred to the emergency department for urgent evaluation and endoscopic management.
Diagnosis and Management
*Once a patient presents with symptoms suggesting a Schatzki ring, the first step in evaluation is a barium esophagram. To completely distend the esophagus, a barium esophagram should be obtained using a full-column technique with a Valsalva maneuver, after swallowing a solid food bolus, while the patient is in either a prone or prone oblique position.
*Endoscopy is often required to confirm the presence of Schatzki ring and rule out other causes of strictures, especially malignancy.
*Differential diagnosis includes eosinophilic esophagitis, reflux esophagitis, esophageal strictures, extrinsic esophageal compression, motility disorders and malignancy. If in combination with chest pain, infectious indications such as candida esophagitis, pill esophagitis, radiation-induced esophagitis or stricture, or esophageal rupture should be considered, especially if the symptoms are acute.
*Management of symptomatic patients includes dilatation of the ring and/or obliteration with biopsy forceps, often combined with acid suppression therapy.
*Recurrence is not uncommon, with rates of up to 64 percent in the first two years. Most of these patients will require repeat endoscopic therapy.

Stacia Sackmaster, APN-BC
Rockford Gastroenterology Associates
Rockford, IL

Corrie Scott, APN-BC
Rockford Gastroenterology Associates
Rockford, IL

Sarah Enslin, PA-C
University of Rochester Medical Center
Rochester, NY

Joseph Vicari, MD, MBA, FASGE
Rockford Gastroenterology Associates
Rockford, IL
Corrie Scott, APN-BC, and Stacia Sackmaster, APN-BC, are family nurse practitioners at Rockford Gastroenterology Associates, Ltd.
Sarah Enslin, PA-C, is a physician assistant (PA) at the University of Rochester Medical Center in Rochester, N.Y., with over 10 years of experience as a practicing PA in GI. Sarah serves on several national GI committees and is a member of the ASGE Practice Operations Committee and ASGE APP Task Force.
Joseph Vicari, MD, FASGE, joined Rockford Gastroenterology in 1997 and has served as managing partner. He previously served as chair of the ASGE Practice Operations Committee and currently serves as councilor on the ASGE Governing Board and co-chair of the ASGE APP Task Force.
References
- Ergun GA, Kahrilas PJ. Esophageal rings and webs. Updated November 3, 2023. UpToDate. https://www.uptodate.com
- Chen YM, Gelfand DW, Ott DJ, Munitz HA. Natural progression of the lower esophageal mucosal ring. Gastrointest Radiol. 1987;12:93-98. doi: 10.1007/BFO1885113
Additional Resources
Haag A. Shatzi ring. What is it, causes, treatment, and more. Osmosis from Elsevier.
https://www.osmosis.org/answers/Schatzki-ring
Watts LD, Patel K. Schatzki ring. StatPearls [Internet]. January 2023. Updated April 6, 2023.
https://www.ncbi.nlm.nih.gov/books/NBK519022/