A 48-year-old male with a medical history for hyperlipidemia and appendectomy several years ago presents to the emergency room (ER) with a chief complaint of nausea and vomiting. The nausea and vomiting began 12 hours ago. He has had multiple episodes of nonbloody emesis. He also describes crampy abdominal pain located around the “belly button” and inability to pass gas (flatus). His only medication is atorvastatin.
Physical examination reveals abdominal distention, tympany on percussion and high-pitched “tinkling” sounds on auscultation. The ER advanced practice provider-physician team suspects an acute small bowel obstruction (SBO) secondary to adhesions from his appendectomy.

A 48-year-old male with a medical history for hyperlipidemia and appendectomy several years ago presents to the emergency room (ER) with a chief complaint of nausea and vomiting. The nausea and vomiting began 12 hours ago. He has had multiple episodes of nonbloody emesis. He also describes crampy abdominal pain located around the “belly button” and inability to pass gas (flatus). His only medication is atorvastatin.
Physical examination reveals abdominal distention, tympany on percussion and high-pitched “tinkling” sounds on auscultation. The ER advanced practice provider-physician team suspects an acute small bowel obstruction (SBO) secondary to adhesions from his appendectomy.
The preferred initial imaging study for most patients suspected of having an SBO is:
A) Upright and supine abdominal films
B) Ultrasound of the abdomen
C) Computed tomography (CT) of the abdomen and pelvis
D) CT enterography
The correct answer is A, upright and supine abdominal films.
Practice Pearls
Plain radiography (upright and supine abdominal films):
Plain radiography is a quick, low-cost, simple, first step to confirm the diagnosis of bowel obstruction. For diagnosis of SBO with plain radiography, the sensitivity, specificity and accuracy are 79 to 83 percent, 67 to 83 percent and 64 to 82 percent.1
Approximately 75 percent of all mechanical bowel obstructions occur in the small bowel.1
Initial imaging should include an upright chest and upright and supine abdominal films. A lateral decubitus can be obtained if the patient cannot be placed in an upright position. This can evaluate for aspiration and pneumoperitoneum and rule out bowel perforation.1
When evaluating abdominal radiographs, it is critical to note patient orientation, as interpretations could differ for images in dependent or nondependent positions.1
Small-bowel versus large-bowel characteristics: a small bowel has circular folds (plicae circulares or valvulae conniventes), is centrally located and appears as thin lines that span the entire diameter of the small bowel. The large bowel has haustral folds that do not span the entire diameter of the bowel.1
Radiological findings of SBO may include: 1
Supine position findings:
- Dilated small bowel > 2.5-3 cm (Image 1)
- Lack of colonic dilation, colon diameter < 6 cm and cecum diameter < 9 cm
- Paucity of colorectal gas
- Stretch sign
- Dilated stomach
- Absence of rectal gas
Upright or decubitus:1
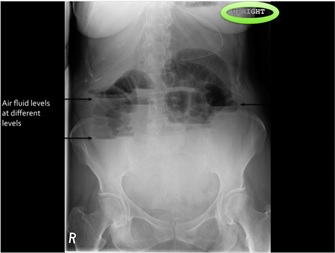
- Multiple air-fluid levels (Image 2)
- Air-fluid level wider than 2.5 cm
- Air-fluid levels in the same small-bowel loop of unequal heights
- String-of-beads sign
(*The greater number of signs present, the higher the specificity for obstruction)
Image 1: Supine abdominal x-ray with dilated small bowel loops
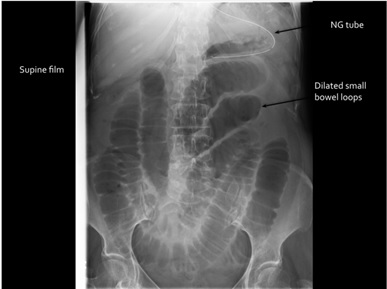
Image 2: Upright abdominal x-ray demonstrating air fluid levels
Free air on plain radiographs indicating bowel obstruction, closed-loop obstruction: U-shaped, distended, fluid filled loops, beak sign presentations.2
If small intestinal ischemia is suspected, abdominal CT should be performed in patients with acute SBO since it is difficult to accurately predict bowel ischemia based on clinical parameters alone.2
Causes of SBO include adhesions, hernias, neoplasm, Crohn’s disease, gallstones, malrotation, duplication cysts, diverticulitis, infection, hematoma, ischemic stricture, intussusception, endometriosis, radiation and foreign body.1
Postoperative SBO after appendectomy is a relatively common complication. Associated risk factors include complicated appendicitis and multiple comorbidities. A laparoscopic approach is less likely to develop adhesions than that of the surgical group.3
Follow-up routine imaging is not generally needed unless the patient fails to improve with nonoperative management at which time a CT scan should be performed.
CT abdomen and pelvis (CT):
- The accuracy of CT in diagnosing acute SBO is >95%.1
- Unless contraindicated, intravenous (IV) contrast should be administered. IV contrast has not been shown to significantly change the sensitivity of CT for the detection of SBO; however, it can improve assessment for bowel wall ischemia.1
- Oral contrast is appropriate and may increase the sensitivity of the diagnosis of low-grade SBO.1, 2
- If high-grade SBO is suspected, oral contrast should be avoided. It does not add to diagnostic accuracy and can delay diagnosis, increase patient discomfort and increase complications, specifically vomiting and aspiration.1, 2
CT findings in acute SBO may include:1, 2
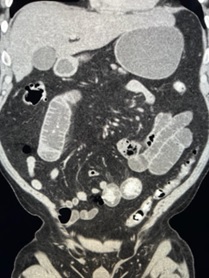
- Dilated proximal small bowel with distal collapsed bowel and air fluid levels (Image 3 and Image 4)
- Proximal small bowel dilation to > 2.5 cm
- Gastric distension
- Bowel wall thickening to > 3 mm (nonspecific)
- Submucosal edema
- Mesenteric edema
Intraperitoneal free fluid is present in approximately one-third of patients with an acute SBO. Free fluid is not necessarily predictive of the need for operative intervention.2
CT has a high accuracy in locating the site of the transition zone in acute SBO.1, 2
*Presence of a transition zone has not been shown to be predictive of the need for operative intervention.2
Image 3: CT abdomen and pelvis demonstrating dilate small bowel and air fluid levels
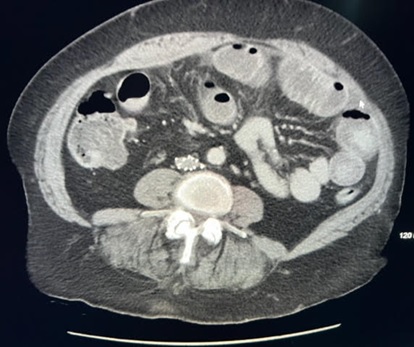
Image 4: CT abdomen and pelvis demonstrating dilate proximal small bowel, dilated stomach and collapsed distal small bowel
All images from the personal library of Robert A. Murray, MD.

Sarah Enslin, PA-C
University of Rochester Medical Center
Rochester, NY

Robert A. Murray, MD
OSF St. Anthony Medical Center
Rockford, IL

Sarah Stainko, MSN, NP-C
Indiana University Health
Indianapolis, IN

Joseph Vicari, MD, MBA, FASGE
Rockford Gastroenterology Associates
Rockford, IL
Sarah Enslin, PA-C, is a physician assistant in the division of gastroenterology and hepatology at the University of Rochester Medical Center in Rochester, NY, with over 10 years of experience as a practicing PA in GI. Sarah serves on several national GI committees and is a member of the ASGE Practice Operations Committee and ASGE APP Task Force.
Robert A. Murray, MD, is a staff neuroradiologist at OSF St. Anthony Medical Center in Rockford, IL. Additionally, he is a clinical assistant professor at the University of Illinois at Chicago, College of Medicine, at Rockford and adjunct professor in the department of physician assistant studies at Marquette University in Milwaukee, WI.
Sarah Stainko, MSN, NP-C is a board-certified nurse practitioner in the division of gastroenterology and hepatology at Indiana University Health in Indianapolis, IN. She works in the area of destination services, innovative endoscopy and motility.
Joseph Vicari, MD, FASGE, joined Rockford Gastroenterology in 1997 and has served as managing partner. He previously served as chair of the ASGE Practice Operations Committee and currently serves as councilor on the ASGE Governing Board and co-chair of the ASGE APP Task Force.
- Nelms DW, Kann BR. Imaging modalities for evaluation of intestinal obstruction. Clin Colon Rectal Surg. 2021;34:205-218. doi: 10.1055/s-0041-1729737. Epub 2021 Jun 2. PMID: 34305469; PMCID: PMC8292005.
- Bordeianou L, Yeh DD. Etiologies, clinical manifestations, and diagnosis of mechanical small bowel obstruction in adults. Updated October 19, 2021. UpToDate. https://www.updtodate.com
- Tseng CJ, Sun DP, Lee IC, Weng SF, Chou CL. Factors associated with small bowel obstruction following appendectomy: a population-based study. Medicine (Baltimore). 2016;95:e3541. doi: 10.1097/MD.0000000000003541. PMID: 27149462; PMCID: PMC4863779.