A 56-year-old male with a past medical history significant for type 2 diabetes mellitus and hypertension presents to the GI clinic with a chief complaint of abdominal pain for four days. Pain is localized to the left lower quadrant. He describes it as sharp and variable in intensity. It does not radiate. He has not had a bowel movement in 48 hours. Typically, he has a bowel movement every day.

A 56-year-old male with a past medical history significant for type 2 diabetes mellitus and hypertension presents to the GI clinic with a chief complaint of abdominal pain for four days. Pain is localized to the left lower quadrant. He describes it as sharp and variable in intensity. It does not radiate. He has not had a bowel movement in 48 hours. Typically, he has a bowel movement every day.
Over the course of the last two days, he has also noted mild urinary urgency. No other symptoms. A colonoscopy three years ago was negative for colonic mass or polyps. He thinks he was told he had “a few pockets” in the colon.
Labs drawn on the day of his clinic visit revealed an elevated white blood cell (WBC) count (14,000). A comprehensive metabolic panel was normal.
His medications are metformin, ASA and lisinopril.
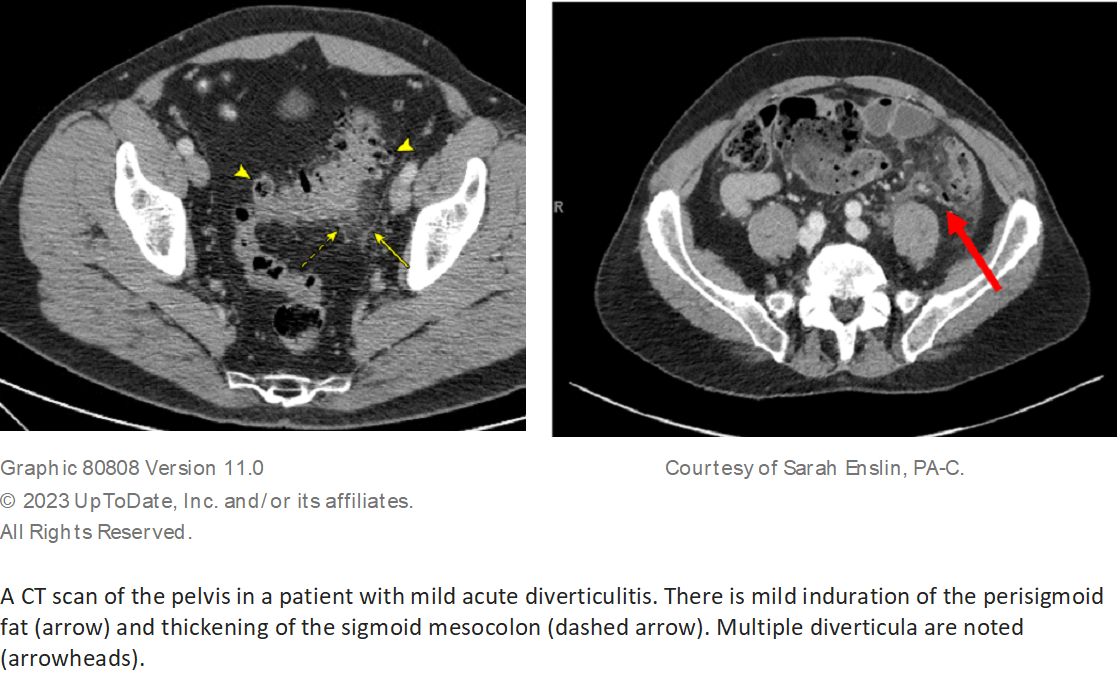
A CT scan of the abdomen and pelvis was performed. Diverticula were present in the descending and sigmoid colon. There was thickening of the sigmoid colon with surrounding fat inflammation (stranding). No abscess and no perforation.
The most likely etiology of his symptoms is:
A) Colon cancer
B) Ischemic colitis
C) Acute uncomplicated diverticulitis
D) Ulcerative colitis
The correct answer is C, acute uncomplicated diverticulitis.
Practice Pearls
The most likely etiology for acute diverticulitis is erosion of the diverticular wall secondary to increased intradiverticular luminal pressure. This results in inflammation and focal necrosis, culminating in micro or macro perforation.1
*Approximately 1% to 4% of patients with diverticulosis develop acute diverticulitis.1 The most common form is acute uncomplicated diverticulitis. Acute complicated diverticulitis is less common (associated abscess, phlegmon, fistula, stricture or obstruction).
*The most common presenting symptom is abdominal pain, typically in the left lower quadrant.1 Change in bowel frequency is often reported with roughly 50% of patients reporting new onset constipation and 25% to 30% reporting diarrhea. Patients may also have urinary symptoms, including urgency, frequency and dysuria.1
*Roughly 20% of patients have a palpable abdominal mass. Patients may have localized guarding, rigidity and rebound.1 Patients may or may not be febrile. Hypotension and hemodynamic instability are rare.1
*Laboratory studies include CBC to rule out leukocytosis (normal in 45% of patients) and C-reactive protein (CRP). Additional labs may include electrolytes, urinalysis and human chorionic gonadotropin in females of childbearing age. Stool studies are only indicated if diarrhea is present, with concern for infectious etiology.
*CT scan with both oral and intravenous (IV) contrast is the examination of choice, with specificity and sensitivity of 94% to 99% when acute diverticulitis is suspected. Findings of acute uncomplicated diverticulitis include localized bowel wall thickening with pericolonic fat stranding in the presence of diverticula.1,2 (Figure 1)
*Colonoscopy is not indicated in acute diverticulitis and should actually be avoided in this setting due to increased risk of perforation. Once the acute attack has resolved (approximately 6-8 weeks), colonoscopy should be done to rule out underlying malignancy if one was not performed in the past year.
*Acute uncomplicated diverticulitis can commonly be managed as an outpatient. Antibiotic treatment can be used selectively rather than routinely in immunocompetent patients with mild uncomplicated diverticulitis.2 Initial treatment in this group consists of pain control and liquid diet. Diet can be advanced to regular as tolerated.
*Antibiotic treatment is advised in patients with uncomplicated diverticulitis who have comorbidities or are frail, present with refractory symptoms or vomiting or have a CRP > 140 mg/L or baseline WBC > 15 x 109 cells per/L.2
*The common antibiotic therapy for acute uncomplicated diverticulitis treated in the outpatient setting is ciprofloxacin 500 mg by mouth every 12 hours and metronidazole 500 mg by mouth every eight hours for 10 to 14 days.3
*Inpatient criteria for acute uncomplicated diverticulitis include sepsis, severe abdominal pain or peritonitis, age older than 70, significant comorbidities, immunosuppression, intolerance of oral intake and failed outpatient therapy.1,2
*If patients meet the criteria for inpatient management of acute uncomplicated diverticulitis, the management consists of intravenous antibiotics, intravenous fluids, pain control and bowel rest (consider a liquid diet).3
*Inpatient antibiotics include Piperacillin 3.375 grams IV every six hours or Ciprofloxacin 400 mg IV every 12 hours with Metronidazole 500 mg IV every eight hours. IV antibiotics are continued until symptoms improve, typically 3 to 5 days, and then patients are transitioned to oral antibiotics once the patient is tolerating oral intake. Total antibiotic therapy (IV + PO) is 10 to 14 days.3
*Discharge criteria include normalization of vital signs, resolution of severe abdominal pain, resolution of significant leukocytosis and tolerance of oral diet.
Figure 1

Katelyn Cookson, PA-C
UCHealth Digestive Health Center
Aurora, CO

Sarah Enslin, PA-C
University of Rochester Medical Center
Rochester, NY
Jennifer Geremia, MSPAS, PA-C
Brigham and Women's Hospital
Boston, MA

Joseph Vicari, MD, MBA, FASGE
Rockford Gastroenterology Associates
Rockford, IL
Katelyn Cookson, PA-C, is a physician assistant specializing in gastroenterology at UCHealth Digestive Health Center and is also an instructor at the University of Colorado Anschutz Medical Campus.
Sarah Enslin, PA-C, is a physician assistant at the University of Rochester Medical Center in Rochester, NY, with more than 10 years of experience as a practicing PA in GI. Sarah serves on several national GI committees and is a member of the ASGE Practice Operations Committee.
Jennifer Geremia, MSPAS, PA-C, is a physician assistant (PA) specializing in gastroenterology, hepatology and endoscopy at Brigham and Women’s General Hospital in Boston.
Joseph Vicari, MD, FASGE joined Rockford Gastroenterology in 1997 and has served as Managing Partner. He previously served as Chair of the ASGE Practice Operations Committee and is currently serves as Councilor on the ASGE Governing Board.
- UpToDate Clinical Diagnosis and Management of Acute Colonic Diverticulitis in Adults. Retrieved from the UpToDate.com website, https://www.uptodate.com.
- Peery A, Shaukat A, Strate L. AGA Clinical Practice Update on Medical Management of Colonic Diverticulitis: Expert Review. Gastroenterology. 2021;160:906-911.
- UpToDate Acute Diverticulitis: Medical Management. Retrieved from the UpToDate.com website, https://www.uptodate.com.