A 54-year-old female with a medical history significant for GERD presents to the GI clinic with a chief complaint of diarrhea. It began six weeks ago. She has four to eight watery, non-bloody bowel movements per day. The diarrhea is associated with fecal urgency and occasional nocturnal diarrhea. She has not used antibiotics recently. She has had no recent travel outside the U.S. or no known ill contacts. She does not use magnesium containing antacids or supplements and denies any recent dietary changes. She does not report consumption of sugar-free candies or diet beverages. Her GERD is well controlled with lansoprazole 30 mg once daily prior to breakfast. Over-the-counter anti-diarrheal medications did not help.

A 54-year-old female with a medical history significant for GERD presents to the GI clinic with a chief complaint of diarrhea. It began six weeks ago.
She has four to eight watery, non-bloody bowel movements per day. The diarrhea is associated with fecal urgency and occasional nocturnal diarrhea. She has not used antibiotics recently. She has had no recent travel outside the U.S. or no known ill contacts. She does not use magnesium containing antacids or supplements and denies any recent dietary changes. She does not report consumption of sugar-free candies or diet beverages. Her GERD is well controlled with lansoprazole 30 mg once daily prior to breakfast. Over-the-counter anti-diarrheal medications did not help.
A complete blood count (CBC), comprehensive metabolic panel (CMP) and stool studies (including Clostridiodes difficile) were negative. A colonoscopy showed normal-appearing colonic mucosa. Random colon biopsies revealed a subepithelial band >10 micrometers.
The cause of her diarrhea is:
A) Crohn’s disease
B) Ulcerative colitis
C) Infectious colitis
D) Collagenous colitis
The correct answer is D, collagenous colitis.
Practice Pearls
Microscopic colitis is a chronic disease of the colon, characterized by chronic, watery, non-bloody diarrhea.1 Microscopic colitis is subdivided into collagenous colitis and lymphocytic colitis.
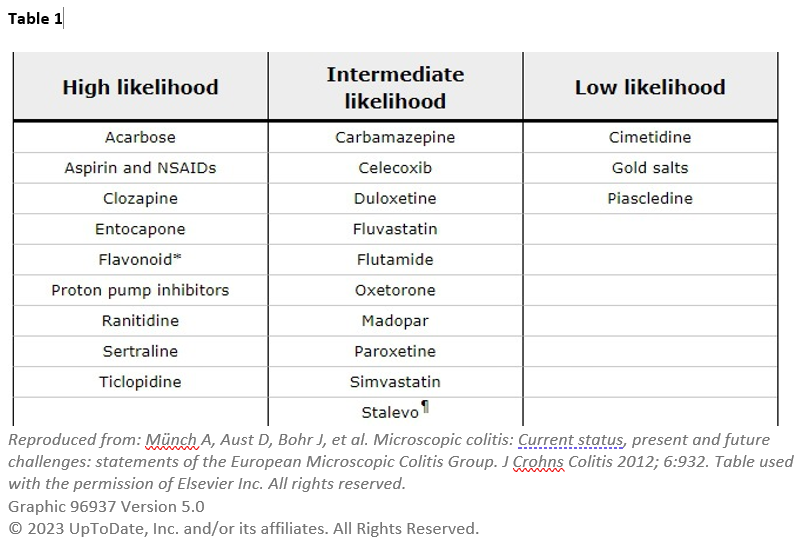
The estimated incidence of collagenous colitis and lymphocytic colitis is 2.0 to 10.8 and 2.3 to 16 per 100,000 per year, respectively.1 Microscopic colitis, especially collagenous colitis, is more common in women. The median age of diagnosis is 65 years. Microscopic colitis is associated with autoimmune diseases (e.g., celiac disease). Risk factors include nonsteroidal anti-inflammatory drugs, statins, selective serotonin reuptake inhibitors and protein pump inhibitors (Table 1).1,2
The pathogenesis of microscopic colitis is unknown; it is likely multifactorial, involving mucosal immune response to luminal factors in a genetically predisposed individual.1 Diarrhea in microscopic colitis is likely secondary to mucosal inflammation and bile acid malabsorption.
It is commonly characterized by chronic or recurrent, non-bloody, watery diarrhea.
Patients usually have four to nine watery stools per day. In extreme cases, patients can exceed 15 bowel movements per day. Diarrhea often occurs gradually; however, 40 percent of patients have a sudden onset.
Associated symptoms include fecal urgency, incontinence, nocturnal bowel movements, abdominal pain, weight loss and fatigue, which can significantly reduce patient quality of life. Extraintestinal symptoms include arthralgia, arthritis or uveitis. Some patients, particularly older patients, may develop acute kidney injury secondary to dehydration from persistent watery diarrhea.
Evaluation of microscopic colitis includes CBC, CMP and stool cultures, including C difficile and celiac serology. Consider testing for ova and parasites if the patient has risk factors.
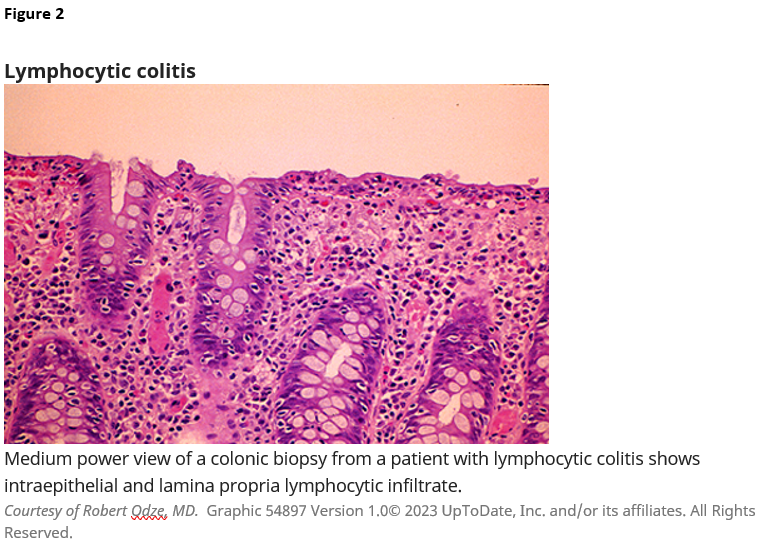
Endoscopically, the colon is typically normal. Histologically, the inflammatory cell response is similar for lymphocytic colitis and collagenous colitis, consisting of mononuclear cells, with few neutrophils and eosinophils in the lamina propria.1
Figure 1: Collagenous colitis-subepithelial band > 10 micrometers
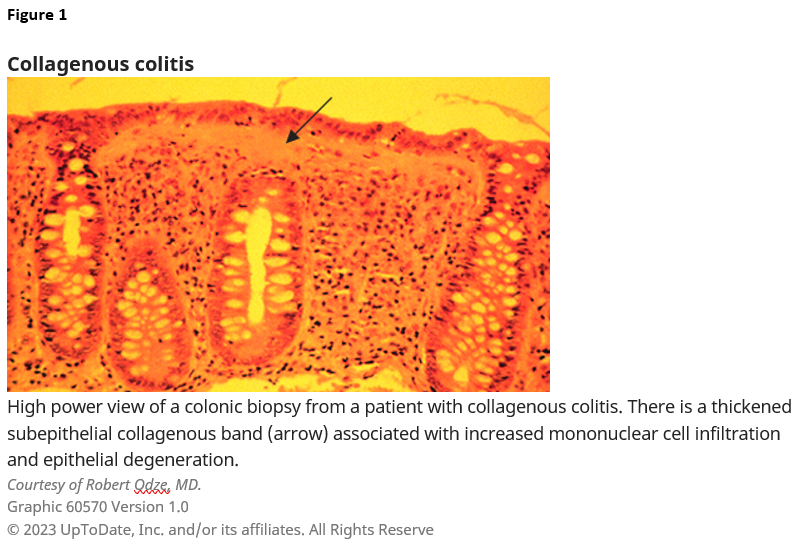
Figure 2: Lymphocytic colitis > 20 intraepithelial lymphocytes per 100 epithelial cells
Most experts recommend performing a colonoscopy with a biopsy of the right and left sides of the colon to reduce the potential for false-negative biopsy results, as microscopic colitis can be patchy in location. However, flexible sigmoidoscopy will diagnose > 90 percent of microscopic colitis.1
Table 1: Recommendations include avoiding smoking and avoiding medications that increase the risk of microscopic colitis, if possible.1
If symptom severity is mild, the first-line treatment is an anti-diarrheal medication, especially for patients with nocturnal symptoms. If diarrhea persists despite anti-diarrheal treatment or if patients have active disease (≥ 3 stools daily or ≥ 1 watery stool daily), budesonide (9 mg once daily) is recommended for 6 to 8 weeks. Budesonide is then gradually tapered in patients with clinical remission (< 3 stools daily or no watery stools).2,4,5
Prednisone is typically considered for treatment if budesonide is not feasible. Cholestyramine, bismuth subsalicylate, biologic agents and immunomodulators can be considered if symptoms persist despite initial treatment.2,4,5
Practical tip: Budesonide can be cost-prohibitive in some patients. In these situations, bismuth subsalicylate 262mg tablets can be used with a dose of three tablets by mouth three times per day.
Relapse occurs in up to 80 percent of patients after tapering off initial therapy. Patients can be maintained on the lowest effective dose of budesonide chronically if needed.

Sarah Enslin, PA-C
University of Rochester Medical Center
Rochester, NY

Palak Patel, PA-C
University of Rochester Medical Center
Rochester, NY

Joseph Vicari, MD, MBA, FASGE
Rockford Gastroenterology Associates
Rockford, IL
Palak Patel, PA-C, is a physician assistant in the Division of Gastroenterology at Northwestern Medicine in Chicago, IL.
Sarah Enslin, PA-C, is a physician assistant at the University of Rochester Medical Center in Rochester, NY, with more than 10 years of experience as a practicing PA in GI. Sarah serves on several national GI committees and is a member of the ASGE Practice Operations Committee.
Joseph Vicari, MD, FASGE, joined Rockford Gastroenterology in 1997 and has served as managing partner. He previously served as chair of the ASGE Practice Operations Committee and currently serves as councilor on the ASGE Governing Board and co-chair of the ASGE APP Task Force.
- Dietrich CF. Microscopic (lymphocytic and collagenous) colitis: Clinical manifestations, diagnosis, and management. UpToDate. Updated July 20, 2022. https://www.uptodate.com
- Fernández-Bañares F, Salas A, Estev M, Espinós J, Forné M, Viver JM. Collagenous and lymphocytic colitis. evaluation of clinical and histological features, response to treatment, and long-term follow-up. Am J Gastroenterol. 2003;98:340-347. doi:10.1111/j.1572-0241.2003.07225.x
- Stewart MJ, Seow CH, Storr MA. Prednisolone and budesonide for short- and long-term treatment of microscopic colitis: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2011;9:881-890. doi:10.1016/j.cgh.2011.06.005
- >Chande N, Al Yatama N, Bhanji T, Nguyen TM, McDonald JWD, MacDonald JK. Interventions for treating lymphocytic colitis. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No.: CD006096. Published July 13, 2017. https://doi.org/10.1002/14651858.CD006096.pub4
- Munck LK, Kjeldsen J, Philipsen E, Fischer Hansen B. Incomplete remission with short-term prednisolone treatment in collagenous colitis: a randomized study. Scandinavian J Gastroenterol. 2003;38:606-610. doi:10.1080/00365520310002210