
A 24-year-old male presents to his primary care physician with complaint of bloody diarrhea x 1 week. Preceding this, he had generalized abdominal cramping and increased frequency of stools for two weeks. He also complains of fatigue and a five-pound unintentional weight loss. He denies fever or chills. He has no known ill contacts. On physical examination, he has mild tenderness to palpation in the left lower abdomen. Labs are notable for iron deficiency anemia (iron = 16 ug/mL, ferritin = 6 ng/mL, hemoglobin = 8.3 g/dL), leukocytosis (WBC = 20,000) and elevated C-reactive protein (CRP = 152 mg/dL). Stool studies were completed and negative for infectious diarrhea. He was referred to the GI office for further evaluation.
Flexible sigmoidoscopy was performed showing marked erythema, loss of vascular pattern, friability and erosions in the sigmoid colon and rectum. Sigmoid biopsies showed severe active chronic colitis with ulceration and crypt abscess formation.
What is the most likely diagnosis?
A) Crohn’s disease
B) Microscopic colitis
C) Ischemic colitis
D) Infectious colitis
E) Ulcerative colitis
The correct answer is E, ulcerative colitis (UC). This patient has severe left-sided ulcerative colitis (ulcerative proctosigmoiditis) with iron deficiency anemia.
Practice Pearls
Clinical Presentation
- Patients with UC often present with diarrhea. Associated symptoms include hematochezia, tenesmus and fecal incontinence.1,2,3
- Symptoms are often progressive and may be accompanied by abdominal cramping, fever, fatigue and weight loss.2
- Physical examination may be normal in patients with mild to moderate disease. In patients with severe UC, patients may have abdominal tenderness, fever, hypotension and tachycardia.1,2
- Extraintestinal manifestations of UC include arthropathy, uveitis, episcleritis, PSC and autoimmune liver disease.1,2,3
Diagnosis
- Labs may show iron deficiency anemia, elevated erythrocyte sedimentation rate, low albumin, elevated CRP and electrolyte abnormalities (from diarrhea/dehydration). Fecal calprotectin may also be elevated.1,2
- Abdominal imaging is not required for the diagnosis of UC.2
- Endoscopic findings (Figure 1) show loss of vascularity, erythema, granularity of mucosa, friability and sometimes bleeding. Inflammation involves the rectum and extends proximally in a contiguous pattern.1,2,3
- Histologic features in UC2,3
- Crypt abscesses, crypt branching, crypt atrophy
- Epithelial cell abnormalities (mucin depletion, Paneth cell metaplasia)
- Inflammatory
changes (lamina propria cellularity, basal
plasmacytosis, basal lymphoid aggregates, lamina propria eosinophils)
Figure 1: Inflamed mucosa in the rectum and sigmoid colon
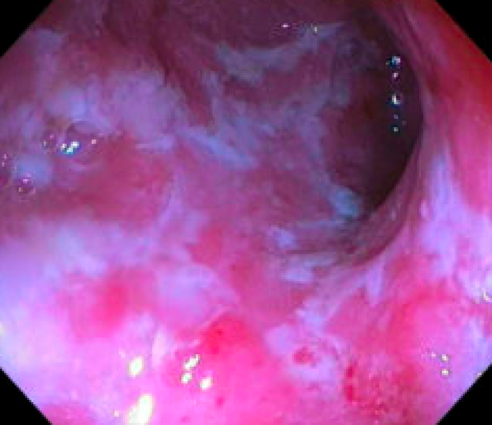
Photo courtesy of Sarah Enslin, PA-C.
Treatment
- Mild to moderate disease2
- Induce remission
- Topical mesalamine
- Topical glucocorticoids
- Oral 5-ASA
- Oral glucocorticoids
- Maintenance therapy
- Topical mesalamine
- Oral 5-ASA
- Moderate to severe disease1,2
- Anti-tumor necrosis factor therapy (infliximab, adalimumab, golimumab) with or without immunomodulator (azathioprine, mercaptopurine)
- Anti-integrin antibody (vedolizumab)
- Anti-interleukin 12/23 antibody (ustekinumab)
- Systemic glucocorticoids
- JAK inhibitors (tofacitinib, upadacitinib)
- Oral sphingosine-1-phosphate receptor modulator (ozanimod)
- Intravenous glucocorticoids
Sarah Enslin, PA-C
University of Rochester Medical Center
Rochester, NY
Jacob Scott, PA-C
University of Rochester Medical Center
Rochester, NY
Sarah Enslin, PA-C, is a physician assistant in the division of gastroenterology and hepatology at the University of Rochester Medical Center in Rochester, NY, with over 10 years of experience as a practicing PA in GI. Sarah serves on several national GI committees and is a member of the ASGE Practice Operations Committee and ASGE APP Task Force.
Jacob Scott, PA-C, is a physician assistant in the division of gastroenterology and hepatology at the University of Rochester Medical Center in Rochester, NY.
- Feuerstein JD, Isaacs KL, Schneider Y, Siddique SM, Falck-Ytter Y, Singh S. AGA Clinical Practice Guidelines on the management of moderate to severe ulcerative colitis. Gastroenterology. 2020;158:1450.
- Cohen RD, Stein AC. Management of moderate to severe ulcerative colitis in adults. Updated September 20, 2023. Accessed at https://www.uptodate.com/contents/management-of-moderate-to-severe-ulcerative-colitis-in-adults.
- Singh S, Ananthakrishnan AN, Nguyen NH, Cohen BL, Velayos FS, et al; AGA Clinical Guidelines Committee. AGA Clinical Practice Guideline on the role of biomarkers for the management of ulcerative colitis.Gastroenterology. 2023;164:344.