
A 24-year-old male presents to the emergency room with a chief complaint of “I can’t swallow.” He states that while eating dinner, chicken suddenly “got stuck, and I could not swallow.” He can swallow saliva; however, he cannot swallow liquids. He has associated mid-chest discomfort. He denies GI bleeding, heartburn, weight loss or any additional symptoms. Over the last two to three years, he has experienced intermittent solid food dysphagia, which has caused him to eat slowly and chew food repeatedly. There are no prior episodes of food impaction. He has a history of seasonal allergies for which he takes an over-the-counter antihistamine. He denies other medical problems.
The most likely diagnosis is:
A) Achalasia
B) Heartburn
C) Esophageal adenocarcinoma
D) Eosinophilic esophagitis
The correct answer is D, eosinophilic esophagitis (EoE).
Practice Pearls
Epidemiology
The prevalence of EoE in the U.S. may vary by region (higher prevalence in the Northeast) and by setting (higher prevalence in urban areas compared with rural areas).1 In Olmsted County, Minnesota, the prevalence was estimated to be 55 per 100,000 in 2006.2
The incidence of EoE is rising in the U.S. A population-based study evaluated the incidence of EoE in Olmsted County, Minnesota, over 30 years. The incidence increased significantly during the last three of the five-year intervals examined, from 0.32 per 100,000 population between 1991 and 1995 to 9.45 per 100,000 between 2001 and 2005.2
EoE is more common in adult males compared with adult females. Symptoms may be present for up to 4.5 years prior to the diagnosis.1
EoE subtypes
- EoE1: mild subtype with normal-appearing esophagus and mild histological and endoscopic changes.1
- EoE2: an inflammatory subtype with highest expression of inflammatory cytokines. Disease may be steroid responsive or steroid refractory.1
- EoE3: fibrostentotic subtype with narrow caliber esophagus, characterized by the highest degrees of endoscopic and histologic severity.1
Clinical Manifestations
Dysphagia to solid food is the most common symptom. A history of acute esophageal food impaction is present in up to half of patients with EoE. 1,3
Patients with EoE learn to compensate for symptoms of dysphagia. The acronym IMPACT may help identify patients with EoE:
- Imbibe (liquids with meals)
- Modify eating habits
- Prolonged (eating very slowly)
- Avoidance (certain foods or social situations during meals)
- Chew (repeatedly)
- Turn away food.4
Esophageal strictures are present in up to one-third of patients.1
Esophageal dysmotility can be seen in EoE. This finding suggests possible eosinophilic involvement of the muscular layers of the esophagus.1 In one study, 15% of patients with EoE who underwent high resolution esophageal manometry had an obstructive motor disorder.1
Additional symptoms of EoE include mid-chest pain, GERD-like symptoms and upper abdominal pain.
EoE is strongly associated with other conditions such as food allergies, environmental allergies, asthma and atopic dermatitis.1,3
Diagnosis
Diagnosis of EoE is based on clinical symptoms (dysphagia, food impactions, odynophagia and chest pain), endoscopic findings, histology and exclusion of other causes of dysphagia.
Endoscopic findings include stacked circular rings, linear furrows, white specks (eosinophil microabscesses) and strictures.1 (Image 1)
Two to four biopsies should be obtained from the distal as well as the proximal or mid esophagus.1 Biopsies reveal esophageal eosinophilia with at least 15 eosinophils per high-power field.1 (Image 2)
Treatment
Initiate full-dose proton pump inhibitor (PPI) orally twice daily for eight weeks. For patients who respond at eight weeks (based on symptom, endoscopic and histologic improvement), continue PPI at the lowest possible dose to control symptoms.6
For nonresponders at eight weeks, consider alternative therapies such as topical glucocorticoids with or without a six-food elimination diet (cow’s milk, wheat, egg, soy, peanuts/tree nuts and fish/seafood). Long-term compliance with the six-food elimination diet is difficult to achieve. Glucocorticoid options include fluticasone 220-mcg spray, two puffs swallowed twice daily for eight weeks or budesonide oral viscous slurry 2 mg swallowed twice daily for eight weeks.5,6
Maintenance therapy with topical glucocorticoids should be considered in patients with severe dysphagia, food impaction, high-grade strictures and rapid relapse.5,6
An option for nonresponders 12 years of age or older (weigh at least 88 lb) is dupilumab. Dupilumab, an interleukin (IL)-4 receptor antagonist, is approved by the U.S. Food and Drug Administration for the treatment of EoE in the U.S. Data show symptom improvement and histologic improvement with dupilumab compared with placebo in both treatment-naïve patients and in patients who have previously tried/failed topical glucocorticoids.1,7
Dilation of strictures can provide symptom improvement for dysphagia; however, it does not improve inflammation. Dilation is typically reserved for nonresponders to medical therapy or high-grade strictures.1,5
Image 11
Endoscopic image of eosinophilic esophagitis

This upper endoscopy in a 36-year-old man with dysphagia shows multiple rings in the proximal to mid esophagus, giving it the appearance of a trachea. Small whitish papules are also visible, representing eosinophilic abscesses on histology. The patient's symptoms responded to swallowed (i.e., topical) fluticasone.
Courtesy of Eric D Libby, MD.
Graphic 51432 Version 4.0
© 2023 UpToDate, Inc. and/or its affiliates. All Rights Reserved.
Image 21
Eosinophilic esophagitis
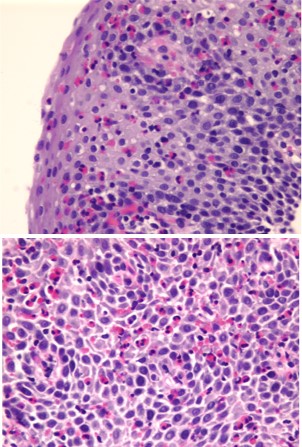
Esophageal biopsies from a patient with eosinophilic esophagitis. There is severe active esophagitis characterized by marked basal zone hyperplasia (top panel) and large numbers of eosinophils (greater than 40 per high-power field; bottom panel). Biopsies obtained from the proximal, mid and distal esophagus showed similar findings. The long linear extent of the esophagitis plus the large numbers of eosinophils are characteristic pathologic features of eosinophilic esophagitis.
Courtesy of Maria Botero, MD and Donald Antonioli, MD.
Graphic 70915 Version 2.0© 2023 UpToDate, Inc. and/or its affiliates. All Rights Reserved.

Sarah Enslin, PA-C
University of Rochester Medical Center
Rochester, NY

Jill Olmstead, DNP, ANP-BC, FAANP
Providence St. Joseph Hospital
Fullerton, CA

Joseph Vicari, MD, MBA, FASGE
Rockford Gastroenterology Associates
Rockford, IL
Sarah Enslin, PA-C is a physician assistant (PA) in the division of gastroenterology and hepatology at the University of Rochester Medical Center in Rochester, NY, with over 10 years of experience as a practicing PA in GI. Sarah serves on several national GI committees and is a member of the ASGE Practice Operations Committee and ASGE APP Task Force.
Jill Olmstead, DNP, ANP-BC, FAANP, is an adult nurse practitioner (NP) at Providence St. Joseph Health. She has practiced as an NP for over 15 years, specializing in gastroenterology. Her practice includes evaluating and managing new patient GI consultations, follow-up visits and diagnostic flexible sigmoidoscopies. She previously served on the ASGE Reimbursement Committee and currently serves as co-chair of the ASGE APP Task Force.
Joseph Vicari, MD, FASGE, joined Rockford Gastroenterology in 1997 and has served as managing partner. He previously served as chair of the ASGE Practice Operations Committee and currently serves as councilor on the ASGE Governing Board and co-chair of the ASGE APP Task Force.
- Bonis PAL, Gupta SK. Clinical manifestations and diagnosis of eosinophilic esophagitis. Updated September 15, 2023. UpToDate. https//www.uptodate.com.
- Prasad GA, Alexander JA, Schleck CD, et al. Epidemiology of eosinophilic esophagitis over three decades in Olmsted County, Minnesota. Clin Gastroenterol Hepatol. 2009;7:1055-1061.
- Eosinophilic Esophagitis (EoE). American Academy of Allergy, Asthma and Immunology. Updated May 1, 2023. Accessed September 20, 2023. www.aaaai.org.
- Hirano I, Furuta GT. Approaches and challenges to management of pediatric and adult patients with eosinophilic esophagitis. Gastroenterology. 2020;158:840-851.
- Bonis PAL, Gupta SK. Treatment of eosinophilic esophagitis. Updated September 6, 2023. UpToDate. https//www.uptodate.com.
- Hirano I, Chan ES, Rank MA, Yngve TFY on behalf of the AGA Institute and the Joint Task Force on Allergy-Immunology Practice Parameters. AGA Institute and the Joint Task Force on Allergy-Immunology Practice Parameters Clinical Guideline for the Management of Eosinophilic Esophagitis. Gastroenterology 2020;158:1776-1786.
- Dellon ES, Rothenberg ME, Collin MH, et al. Dupilumab in adults and adolescents with eosinophilic esophagitis. N Engl J Med. 2022;387:2317-2330.