 Evolving patient care needs, physician shortages, and operational challenges during the COVID-19 pandemic have highlighted the importance of optimizing our healthcare delivery teams. Advanced Practice Providers (APPs) are indispensable members of the healthcare team and are increasingly being utilized in all practice settings. The role of the APP varies based on state/institutional policies, departmental/practice needs, APP qualifications, and physician scope of practice. Despite these variables, incorporating APPs into specialty practices has been shown to improve access to and timeliness of care without compromising quality of care.1
Evolving patient care needs, physician shortages, and operational challenges during the COVID-19 pandemic have highlighted the importance of optimizing our healthcare delivery teams. Advanced Practice Providers (APPs) are indispensable members of the healthcare team and are increasingly being utilized in all practice settings. The role of the APP varies based on state/institutional policies, departmental/practice needs, APP qualifications, and physician scope of practice. Despite these variables, incorporating APPs into specialty practices has been shown to improve access to and timeliness of care without compromising quality of care.1
The US Bureau of Labor Statistics report Physician Assistants (PAs) and Nurse Practitioners (NPs) to be two of the fastest-growing occupations.2,3 The increased demand for healthcare services and the exponential increase in APPs necessitate a leadership structure that will clearly define the scope of practice and performance expectations that align with national, state, and institutional requirements. Recognizing APPs as providers and utilizing them in roles that allow them to work to the fullest extent of their licensure is essential in creating high-functioning healthcare teams, optimizing the allocation of resources, and reducing duplication of work. Underutilization can lead to decreased revenue, decreased APP satisfaction, and decreased retention.
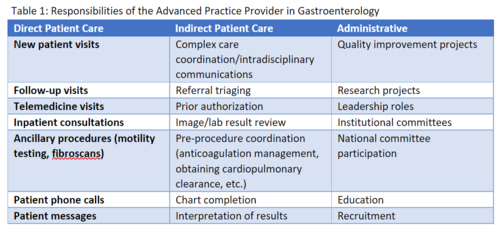
In addition to being at the forefront of patient care, APPs are also involved in many tasks associated with indirect patient care and administration. These are summarized in Table 1. It is important for practices to recognize these additional responsibilities and define performance metrics that account for the RVU-generating and non-RVU generating tasks. A designated reporting structure clearly defined administrative support, and standardized scheduling templates are also essential to maximize workflow efficiency. This is best accomplished by including APPs in team meetings and leadership roles. As team members involved in direct and indirect patient care and administrative duties, APPs are key members of the GI team and can provide valuable input to improve clinical operational efficiency, participate and lead quality improvement projects, and serve as an invaluable resource.
References
-
Tapper EB, Hao S, Lin M, Mafi JN, McCurdy H, Parikh ND, Lok AS. The Quality and Outcomes of Care Provided to Patients with Cirrhosis by Advanced Practice Providers. Hepatology. 2020 Jan;71(1):225-234. doi: 10.1002/hep.30695. Epub 2019 Jun 21. PMID: 31063262; PMCID: PMC6834870.
Sarah Enslin is a Physician Assistant at the University of Rochester Medical Center in Rochester, NY. She graduated from the Rochester Institute of Technology and has over 10 years of experience as a practicing PA in GI. She is the Advanced Practice Provider Manager for the University Medicine Service Line and Co-Lead Advanced Practice Provider for the Division of Gastroenterology & Hepatology. In addition to her administrative responsibilities, she has a busy clinical practice with a special interest in hepato-pancreaticobiliary disease & GI-Oncology. She routinely lectures at the Rochester Institute of Technology PA Program and is a sought-after speaker regionally and nationally. She also participates in clinical research projects and is a preceptor for APP students from four different colleges and universities in the Upstate NY region. Sarah serves on several national GI committees and is a member of the ASGE Practice Operations Committee. She has several peer-reviewed publications to her credit and regularly presents at national meetings.